tv Democracy Now LINKTV December 6, 2012 3:00pm-4:00pm PST
3:00 pm
3:01 pm
the centers for disease control and prevention in atlanta, georgia, thency responsible for monitoring the health status of the american people. stephen ostroff: cdc functions as the doctor for the community or for the public at large, and so we monitor health status in a much broader sense. our job is to watch the health of the american public, and when we see disturbances in the health of the american public, when we see diseases, our job is to try to figure out why they occur and how to both control them-- but more importantly, to prevent them. people often ask why this large public agency is located in atlanta instead of the nation's capital.
3:02 pm
we are the only major government agency that is not headquartered in washington, dc, and both the fact that we're not in washington as well as the date that we were established, tells you something about our history. in 1946, troops were returning home from europe and the pacific after world war ii. the joy of their return was tempered by public health concerns about what might be arriving with them. would their homecoming also reintroduce diseases that had been erased from the national scene? in the southeastern part of the united states, up until well into the 20th century, this was an area that had malaria. there was a lot of concern that as soldiers returned from areas, particularly in the pacific, which were high-incidence areas for malaria, that as they came back to military bases in the southeast, that there was a possibility
3:03 pm
that they would reintroduce malaria into the mosquito populations around those military bases, and so a little unit was established in atlanta, being that it was the largest city in the southeast, to make sure that those mosquito populations were kept under control around the military bases, so that malaria wouldn't come back in this part of the country. and the way you control it, and the way we did in this country, was you got to get rid of the mosquito vector. that takes a sophisticated... well, it takes an organized community effort. the chinese did that in southern china. many places around the world have had malaria problems-- brazil-- that they've brought under control. not so in africa. eradication efforts are erratic. yellow fever is another mosquito-transmitted virus that the french encountered when they occupied west africa. so the way the french dealt with this
3:04 pm
was to conduct an ongoing every-four-year campaign to vaccinate every person in every country they occupied. they had groups of doctors and nurses--that's all they did. they just went from village to village on this four year cycle. that way, the most that could happen is you'd have a group of susceptible children, but it would never get very big before you'd be through vaccinating the next time around. that way, they kept yellow fever under control. now, when those countries became independent, there wasn't money for those programs. and i got introduced to yellow fever in africa because, in 1965... some seven or eight years after senegal got its independence, there was a big epidemic of yellow fever, and it was all in children under 10 years of age,
3:05 pm
because they hadn't been vaccinated. when we started off at cdc, a lot of emphasis was on infectious diseases. that's really how cdc grew. but at the same time, i think there was a general feeling that infectious diseases were really conquered. it was really sort of a mopping up operation that we were about. the fact that malaria had disappeared from the united states, and we conquered smallpox in the americas in 1971 and worldwide in 1977, sort of lent us confidence that really, there wasn't much that we couldn't do. as a result, the center began to diversify, to broaden its focus. and so we expanded into chronic disease areas. the national institute for occupational safety and health was incorporated into cdc in the early 1970s. much more recently, we've gotten into areas surrounding injury control and prevention. and of course we realized in the last few years
3:06 pm
that the infectious disease agenda is not over. certainly it's not in the developing world where it still causes a very heavy burden. apart from what aids is doing as probably the most egregious example that we've seen in our lifetimes, having surpassed malaria as the largest killer of people in africa, is tuberculosis, for which we've had good drugs, haven't used them wisely or enough in years past to reduce some of the problems that we're seeing today. and that's getting more and more serious now with multiply resistant strains of tuberculosis. tuberculosis is the most common infectious agent worldwide, and that has not changed. that is, of course, particularly true in developing countries, and particularly in asia, where the burden of tuberculosis is heaviest. in a number of the industrialized countries-- and the united states is perhaps the best example-- we've had tremendous success in controlling tuberculosis and did so up until the sort of mid-1980s, and then, due to a number of factors--
3:07 pm
some complacency, declining resources directed at tuberculosis and other illnesses we assumed were going to disappear, lack of sort of attention by the public health community-- tuberculosis came back, and came back somewhat slowly, subtly, until we realized we had a serious problem. we were victims of our own success. we had all these wonderful antibiotics, we had wonderful, very safe and effective vaccines that took care of polio and that got rid of smallpox and that largely got rid of measles, and there sort of became a perception that, why do we need to spend all this money? why do we need to have all these people to take care of problems that don't exist anymore? and so the resources got shifted away, both out of health-- but within public health, into other areas of public health. this was the period when the chronic disease activities were picking up. this was also the era of aids,
3:08 pm
and a lot of the resources that were being used for other communicable diseases got shifted over to try to deal with the aids problem. and so we watched the infrastructure erode to the point where the local and state health agencies couldn't do their normal baseline functions to monitor-- what we consider the essential role, which is to monitor the pulse of the health of their populations. david bennett: in some marginalized populations and in people in jails and prisons, we found we had a big challenge on our hands, and there was a wake up call, a good response, and i think we've now turned the corner, but hopefully, we've learned our lessons, that the fact that we're now seeing a decline in tuberculosis doesn't give us any guarantees for the future. another thing that haunts me is, now, there are other much more common problems such as measles and some of these other ones for which, in the case of measles, we've had a perfectly good intervention now
3:09 pm
for more than 30 years and have not used it. we're using it more and more now to help reduce it, but there are several other problems. measles, polio, mumps, and chicken pox. the vaccine-preventable diseases of childhood are rarely seen in the industrialized nations of the world because of the immunization programs that exist. david bennett: measles is still a serious disease in many developing countries, especially in africa and in many countries in asia. even in healthy populations, measles will kill on an average of one per thousand children who are infected with measles, and if you don't immunize, every child would eventually get measles. it's even more serious in african populations where one has other illnesses and malnutrition at the same time, and that means children are quite likely to die, even 10% of children who get measles. in the next few years, the world health community will be targeting measles for eradication. it is next in line after polio.
3:10 pm
we need to approach diseases individually, where we have specially selected diseases that are amenable to a concentrated attack, to bring them to eradication. there's no substitute for that. the cost/benefit of getting rid of a disease is very high, often infinite, depending on how far you want to calculate it out. the issue of disease eradication is a very interesting one. the only example that we currently have is smallpox, where we know that the only reservoir in nature for smallpox was humans. and so, if you could break the chain of transmission in humans-- and it wasn't a latent infection in humans, and so it caused an acute disease, and then it disappeared-- if you could break the chain of transmission in humans, you could eradicate the disease. there hasn't been a case of smallpox that's occurred anywhere in the world since 1977, and so we're now more than 20 years out,
3:11 pm
and so i think we have a fair degree of confidence that we have eradicated the disease in nature. the only known repositories of the smallpox virus are here at the centers for disease control and prevention, and also in equivalent institutions in russia. of course, one of the more active discussions that's gone on over the last couple of years has been whether or not those stocks should be destroyed in order to ensure that any opportunity for this to break out of those laboratories and get back into the population is reduced to zero as much as conceivably could be. the counterarguments to that, of course, is number one-- you'd be destroying a living species. the other is that you never know when you may need the live virus to be able to do research. one of the interesting things about smallpox is you don't need the virus to make the vaccine. the vaccine is a different virus. it's cowpox. and so you can produce lots of smallpox vaccine without needing the virus itself.
3:12 pm
the other interesting component of the smallpox story is that the fact that the disease has been eradicated and the fact that we stopped vaccinating the populations has made it a potentially very desirable bioterrorism agent. it's a highly transmissible illness. the levels of immunity in the population, not only of the united states but everywhere else in the world, is quite low. the world community will face similar questions once polio and measles are eradicated. with measles and with polio, the story is much more complicated, because you do need the viruses to make the vaccine. in recent years, a strike force of deadly microbes has taken aim at the world. because these bacteria and viruses multiply quickly, they evolve rapidly into even more aggressive strains. most people, when they think of these emerging infectious diseases, think about them happening in sudan, or in the middle of africa, or in the middle of the remotest parts of asia or wherever, and we have to realize that if we look down the list
3:13 pm
of diseases and pathogens that we've discovered over the last 20 to 25 years, just as many of them have been found right here in the united states as has been found elsewhere in the world. often a new pathogen is discovered when there are simultaneous outbreaks of an illness that can't be explained. this is a red flag to the centers for disease control. and e. coli 157 actually fits into that mold. when there were near-simultaneous outbreaks, one of them in southern oregon, the other one in... the upper part of the lower peninsula of michigan. there were suddenly a large number of people in relatively small communities with very severe, bloody, diarrheal illness. and when these people went to their health care providers, the health care providers took specimens, tested them for the bugs that they knew caused that type of bloody diarrhea and came up with nothing.
3:14 pm
they turned first to the local, then to the state public health department, and when that didn't turn up any answers, the state asked the cdc for assistance. and so in circumstances where people can't come up with the causative agent, those specimens can then come into our laboratories, and we can run tests for a variety of different things that are both known and unknown. and that's what we did in that particular situation. and one of the things that we noticed is that we found that there were unusual e. coli in several of the specimens that were submitted to us from both oregon and from michigan. now, everyone normally has e. coli in their g.i. tract. it's a normal inhabitant, and you need it to break down certain foodstuffs to be able to absorb them, and this was not an e. coli that was recognized to be one of the bad ones. we further tested it, and we discovered that it had some unusual features
3:15 pm
that hadn't been seen before. with many of the emerging infectious diseases that we've seen, we can tell retrospectively that they're not really new. they're just newly recognized. the cdc and its counterparts in canada and great britain describe themselves as pack rats when it comes to specimens. we save everything, and if you go around our laboratories and you look in the freezers, you'll find all kinds of stuff that we've collected over the last 50 years. and we went back into our inventories, looking to see if we had old ones of this e. coli 157 in our collections. the canadians did the same things, the british did the same things in their inventories. in the case of this e. coli, it genuinely appears to us to be a new one. it looks like it's a bug, it's been around for some period of time. it sort of got together in the wrong neighborhood with some other bad players and picked up some of its bad habits. basically, what happened is that some of what we call virulence factors got picked up by this bug from other bugs
3:16 pm
and then turned what was probably a fairly harmless e. coli into one that causes a fairly severe illness-- not only the bloody diarrhea, but also some complications with-- affecting kidneys, particularly in very young children. the risk factor for the disease, discovered in both the oregon and michigan outbreaks, was a large cheeseburger that people had ordered from the same fast food chain. we then continued to search, because at that point, it wasn't clear to us whether this was just a very unusual occurrence and we weren't going to see this again, or whether or not we were genuinely looking at sort of a new major emerging disease in north america. and so we searched very diligently over the next couple of years for outbreaks. we found a small number of sporadic-- for us, sporadic means a case here and a case there but not part of a larger, recognized outbreak-- and we actually did investigate one or two other outbreaks.
3:17 pm
there was one that was in nebraska, in a nursing home, where it turned out hamburgers were also implicated. but then, in the 1990s, a major outbreak did occur. stephen ostroff: and that of course was a very large outbreak that occurred in the pacific northwest linked to jack in the box which involved somewhere in the range of 700-800 people with a number of deaths, and for want of a better term, it sort of put this bug on the map. we've learned over the years that primarily th is a bug that lives normally in the gastrointestinal tract of cows and is quite happy there and doesn't cause any disease. and so many of the problems that we've seen with this have been related to both dairy products as well as ground beef. but in addition to that, its sort of spectrum of implicated food items has expanded over the years, particularly into fruits and vegetables.
3:18 pm
as we look at this, it seems to be related to farming techniques that might allow access of cow manure into things where we would think that it shouldn't be. we have worked very closely with the regulatory agencies that are responsible for trying to reduce the occurrence of this in both meat products as well as other items-- the food and drug adnistration and the department of agriculture-- to implement measures that we believe would work to reduce its presence in the food products in the country. the detective work required to identify and counteract a new disease agent like e. coli 157 demands enormous cooperation, not only between the public and private sectors, but among the nations of the world. to do our job, to recognize... the patterns of disease and to recognize anomalies
3:19 pm
from the normal patterns of disease-- because anomalies from the normal pattern of disease are basically what the definition of an outbreak is-- that requires a very tight partnership and working relationship between the clinical community, the health care providers themselves, as well as the laboratories that see the specimens and make the diagnoses. in addition, it requires having robust investigative capacity at mostly the local level, but also at the state level, because by and large, that's where most of the action occurs. it is very, very important, particularly for people in the united states and other relatively wealthy countries to understand that this is one small boat. and we may be in the more affluent part of the boat, but we're still in the same boat, and it's in our interest to help everybody understand their health and deal with their health problems,
3:20 pm
especially the infectious disease problems. the importance of international awareness and coopation even extends to our food supply. one of the things that's happened over the last couple of decades is the significant globalization of our food supply. you know, if you go to basically any nice restaurant in the country and have a several course meal, you could probably count up the number of continents that the various foods on your plate may have come from. the distribution of pathogens that might occur in... peru, or that may occur in... costa rica, is significantly different than might occur in california or in michigan. and so we have to be aware that there are potentially different... risks in terms of those foods. the other is that we've figured out a way to mass produce and mass distribute foods in a volume that we've never been able to do re. and we have a variety of new food products-- prepackaged salads--
3:21 pm
and while in general these products are quite safe, the problem is that if something does go wrong, it can go wrong on a very large-scale basis. the traditional outbreak that we think about-- the bad potato salad at the church supper, you know-- still does occur, but what we see more and more of is we see very low levels of contamination in a product that may be distributed very widely in a large number of states. in order to get a handle on these widely dispersed cases, the cdc is turning to technology. one of the ways that we've been doing that is similar to what the fbi does in terms to having a national database of fingerprints of criminals. anytime one of those bugs is isolated, either from a human stool sample or from a food product, what happens is it goes into a network of laboratories that are capable of performing the fingerprints,
3:22 pm
using standardized methodology. changes in how food is grown and handled, increased international travel, people crammed togethe in uanitary nditions-- all contribute to the emergence of these new and deadlier microbes, but there is another critical factor. david bennett: we now have the threat that our major tools, the antibiotics that we can treat bacterial infections, are being compromised. there's a lot of resistance to antibiotics, both in hospitals and communities, so we're very worried about what will happen there. and this means increased cost, and it also means in some cases we can't effectively treat some infections, or it's much more difficult to treat. stephen ostroff: so rapidly we have watched one after the next after the next of the easy-to-use, cheap, effective antibiotics sort of get thrown by the wayside because of the way that we have indiscriminately and inappropriately used them
3:23 pm
to the point now where as we speak, penicillin basically treats almost nothing. and so my message is-- in terms of emerging infectious diseases-- that the public at large should do what they can do to reduce the likelihood that we will continue to see the spread of antibiotic resistance by only taking those antibiotics when it's appropriate to do so, to not seek antibiotics from your health care provider when you have sort of the usual cold or viral infection that won't be responsive to them. importantly as well, if the doctor tells you to take three tablets a day for seven days or for ten days, and you start feeling better after a day or two, then don't go down to two a day and then don't go down to one a day and then stop taking them after three or four days because you feel all better because that's how you leave behind the resistant bugs. in an effort to stay at least one step ahead of the bugs, the centers for disease control and prevention have started what they call
3:24 pm
the unexplained deaths project. instead of waiting for a doctor to report an illness to the health department, the health department actually goes out and looks for the occurrence of deaths or very severe illnesses where the clinicians think that these are somehow related to some infectious disease but can't figure out what the cause is. and what we do is we collect specimens, both those that are available before the person died, and then post-mortem, we also take what specimens are available, and we run them through a variety of different laboratories, not only here at cdc but also in various academic centers around the country, using the most up-to-date razzle-dazzle technology to see if we can pick up something that is unexpected, that we didn't know was there. for example, the hantavirus, a severe illness that kills four of every ten of its victims, occurred so infrequently that no one picked it up. we know that those cases were going on for decades,
3:25 pm
and nobody ever pieced it together because they were so sporadic and they were so spread out over a geographic area that nobody recognized the patterns. we think that if we had been doing a project like this in 1993, that we would've picked up the existence of the hantavirus before it found us by producing an outbreak. so this is our opportunity to try to get sort of a little bit ahead of the curve and find the pathogens before they come and find us. awareness is important, but just how much time should the public at large worry about e. coli 157 or hantavirus or any of the other deadly pathogens that may emerge? if i was joe public, i wouldn't lose sleep worrying about being the victim of ebola, sitting in kansas city, missouri. i like to say that there are emerging infectious disease problems that we have right here in the united states,
3:26 pm
that you as the public can actually do something about, by taking the necessary prevention and control measures to reduce your individual risk of being the victim of one of these diseases. the types of things that we think about are the vaccine-preventable diseases. we know that a large proportion of the populations that we target to get the flu vaccine-- and we know that influenza kills many more people in the united states than will ever have been recognized with ebola in the world up to this point every single year, and yet we have a very simple preventative, such as the flu vaccine-- over half of the people that are targeted to receive it don't get it. the same itrue of theneumonia vaccine which prevents illness due to a pathogen that's called the pneumococcus. and one of the problems that we've had over the last several years is that this bug has very rapidly developed resistance
3:27 pm
to many of the common antibiotics that are used to treat it. we have a very good vaccine against this particular organism, and yet in the targeted populations-- in elderly individuals and people with chronic lung disease and people with chronic heart disease-- in some of these populations, less than one in five who should get this vaccine-- and you only have to get it once-- actually get it, and so that's a very simple preventative measure that one can take to reduce their risk of being the victim of one of these emerging infectious diseases. similarly, in the whole area of food-borne illness, we know that there are very simple things that one can do, such as kitchen hygiene, such as refrigeration, such as properly cooking your foods and properly washing your foods, which would reduce your individual risk of being the victim of the e. coli bug, and yet it's very hard to get that message across to people. similarly, outdoor activities. you know, insect repellents. we just had this big outbreak in the new york city metropolitan area
3:28 pm
related to this virus that we'd never se befor in the western hemisphere, known as the west nile virus. there were very simple preventative measures that people could take to reduce their risk of being the victim not only of that one but other mosquito-borne diseases, the same with tick-borne diseases. and so, in your own personal campaign against marauding germs and microbes, the advice is clear. concentrate on the things you can do something about, and try not to worry about the rest. "the human condition" is apart series for more information on this ogram, and accompanyingaterials, call or, visit us online at:
3:30 pm
ple and accompanyingaterials, call to aids in this country, in our borders, than all of our world wars. death was a constant in my life for many years. i was sitting by deathbeds day by day, watching people die from the same thing i had. no matter how effectively we work to kill h.i.v., to get rid of it, to vaccinate against it, unless we look hard and carefully at our sexual behaviors and at the entire issue of drug abuse in the world, we will not be over this problem. there will be another epidemic, and another, and another.
3:31 pm
3:32 pm
some cases of severe immune deficiency and fatal infections were reported among gay men from california. the person who was delivering mail to my office didn't show up one day. i said, "where's jose?" and they said, "well, he's hospitalized. he was hospitalized last night. so i went over to see him. he was in a ward two wards over, and he had already died. i said, "but he wasn't sick." and then people started dying within 24 and 48 hours all the time. we were in fact dealing with some of the sickest individuals that i've ever come across. these were typically young people, usually young men in the prime of their lives who were developing severe illnesses, many of which we had no treatment for. steve pieters: as i was pastoring the metropolitan community church of hartford, connecticut, and in 1981, we began hearing stories of this new gayancer and gay men getting a strange form of pneumonia.
3:33 pm
when i started getting sick in 1982, they still weren't quite sure what to call it. they hadn't discovered the virus. they could tell my immune system was severely deficient, but i didn't have any of what were then the five defining diseases of aids. well, the most important thing in investigating a new disease outbreak is to determine, in fact, is it really a new disease outbreak? is the disease new? is it occurring with greater frequency? who's affected by it, and where will it go? what are the horizons of the epidemic, if it's an epidemic? so the most important thing for us initially was to construct a case definition for what is now called aids. so it was decided that we would define aids on the basis of certain illnesses that were never seen in normal people that must somehow be part of this epidemic.
3:34 pm
some of them were these opportunistic infections, some of them were very strange cancers, and, at that moment, there was a line that was drawn. i was so very sick in the first two years. i had hepatitis and cmv and pneumonia and mononucleosis, herpes, shingles, a variety of fungal infections, candidiasis, wasting. i was really sick, and a lot of people in my life thought i was faking because the doctors weren't coming up with a diagnosis. i felt so abandoned and so alone and so scared of what they might say to me, what they might diagnose me with. but between '81 and '83, the case definition was discovered, and the modes of transmission were determined to be through sexual contact primarily, between injection drug users, through the blood supply, and from infected mothers to their children.
3:35 pm
there was already determined to be a risk to healthcare workers, albeit an infrequent one. and transmission through casual contact was ruled out as being a major threat. at the beginning of the epidemic, fear was the bottom line, particularly among health-care providers. and the doctors were, in fact, in a difficult position. on the one hand, we know this is our job. throughout the whole history of medicine, if there was plague, doctors were going to get plague. in the era of antibiotics, we forgot that. early on in the aids epidemic, there were staff, and unfortunately some doctors, too, at that time, who wouldn't even enter the room of a patient with aids. i remember seeing people where they were putting the tray at the side of the bed, at the side of the door. "uh, your food is here." well, the person was too sick to get the food. i mean, it was all-- it was ridiculous.
3:36 pm
steve pieters: here they were telling me that i had the worst possible disease, horribly stigmatized. people were terrified of being around a person with aids back then, and i was left alone a lot. and it was a horrifying experience in every way. there are still nurses, dentists, doctors, surgeons who are unwilling to take care of these patients. as i go around the world and see a beginning of an epidemic in other areas of the world, i see the exact same prejudices that we dealt with 15 years ago. initially the general public was complacent, lulled by the fact that many people considered the virus a "gay" disease. wrong. we should have just said this is a sexually transmitted disease, and if you having sex unprotectedly with more than one--your partner that you're going to be with
3:37 pm
for the rest of your life, then you at risk for h.i.v.-- for aids. we could have saved a lot of lives. they used to tell us at cdc that our public opinion, or public attitude was like a rheostat, that when people were complacent, we would put out information to turn up the heat. when they became too scared, we would put out reassurance. and we had to reassure people that following good scientific studies, that there was no evidence of transmission of the virus through mosquitoes, that there was no risk of getting aids from donating blood, and to get people to focus on what the real risks were. at this point, researchers had pieced together parts of the puzzle-- a definition of the disease and its mode of transmission-- but not identification of the virus itself. in the entire history of medicine, there has never been such a rapid response and such a rapid understanding of what this disease was-- the virus--
3:38 pm
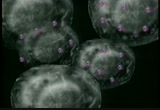
using technical means that were not possible five years before or ten years before. so using the technology that was available in 1981 and 1983, the virus was found. when the virus was discovered, though, what also was discovered was the widespread prevalence of h.i.v. in the united states. from several thousand cases of aids, we learned that there were literally hundreds of thousands of people infected-- indeed, millions throughout the world, already infected. what is this virus known as h.i.v., and what makes it so deadly? h.i.v. stands for human immunodeficiency virus. number one-- virus. that's what it is, not a bacterium. number two-- it causes immuno-deficiency. that means a weakness of the immune system. "human" is because the only species
3:39 pm
that can be infected by that virus and get ill is man and woman, not any other species. once the virus gets into the bloodstream, either directly-- from an infected bit of blood from a needle or a blood transfusion-- or through sexual secretions, the virus immediately starts to divide in this extremely rapid way, a billion new copies every six hours. the virus attaches itself to the t4 cell-- the cell that regulates the body's defense system-- and destroys it. in so doing, it's destroying all of your ability to mount a defense against any other germ that might come along or any cancer cell that might come along. but that's not all. because h.i.v. is a retro virus, it can also insert its genetic material into selected t4 cells.
3:40 pm
alexandra levine: and as long as that t4 cell lives, the virus is living also inside of it. we used to think that if we can just keep the virus hidden in the dna there, then eventually those t4 cells will die out and we might be able to cure this. but it turns out that those long-lived "latently infected" t4 cells in which the virus is there, hidden in the dna, they may live 20 or 30 years, and therefore, the ability to really cure this infection may not be possible. ronald mitsuyasu: so it's a very insidious virus that attacks human immune cells, integrates within the cell itself, and then replicates within those cells and then goes on to attack additional immune cells. and the terrifying thing about h.i.v. is that...
3:41 pm
the patient really does not have an immune response to the virus, and the virus kind of makes sure that it won't be attacked by actually destroying immune cells. at the end of about 10 years, the body just can't keep up anymore, and as the virus infects more and more t4 cells and destroys them, the person begins to get ill. that period of funny little kind-of-ordinary infections goes on for a year or two. after that, the patient will develop a very serious infection of some sort, and those are called opportunistic infections. those are aids-defining illnesses. and when they finally diagnosed me with kaposi's sarcoma, lymphoma, and aids in '84... they told me, "we have nothing we can do for you. there are no treatments." and i came home and gathered friends around me and completely lost it.
3:42 pm
i mean, i burst into tears, i wept, i sobbed, i got angry, i got scared, i got depressed. i felt all those feelings that i'd been scared of feeling up to that moment. and i really let go into it because i knew there were some very loving people around me to support me through it. in 1987, the very first anti-h.i.v. drug was developed. and it may not seem like a big deal, but prior to 1987, we had no antiviral drugs at all. steve pieters: dr. levine offered me the opportunity to be patient number one on the very first drug they ever tried against h.i.v., and i was treated with that drug for a total of 39 weeks. well, within six weeks, all of my kaposi's sarcoma lesions had disappeared. and the lymphoma had gone into complete remission. of the 90 patients who received the drug, steve pieters was the only one to experience positive results,
3:43 pm
along with some unpleasant side effects. it was an extraordinarily toxic drug, and it blew out my adrenal glands. it caused major neuromuscular damage, wasting, peripheral neuropathy. it took me about a year to recover from the side effects of the drug. the other patients have all since died from the progression of aids. it was within the next year the drug azt was introduced. and it was a good drug. it still is. the problem, though, is that if we use one drug to treat the h.i.v. virus, it will absolutely learn how to live with that drug. it becomes resistant to the virus. in a biologic sense, the virus must stay alive. survival of the species, just in the same way that we have to stay alive. and if we give the drug that will kill the virus, the virus is going to have to learn to find a way to live with it, and it did.
3:44 pm
ronald mitsuyasu: within the last five years, the pharmaceutical industry and researchers at various institutions have developed new drugs, more potent antiviral drugs which, in combination with drugs that already existed, allow patients to live for decades. as an example, in the united states, new opportunistic infections went down by 73%, and the death rate from aids went down by essentially 5 50% in one year alone because of access to those drugs. but these drugs are not perfect, and in fact, patients will become resistant to our current antibiotics. so what we have as a challenge to researchers is to find ways of outsmarting the virus using new approaches-- either genetic therapy, immunologic therapies, developing new antibiotics-- new approaches to try to better control the virus
3:45 pm
and allow patients to live with their infection without developing the complications of aids. alexandra levine: they, by necessity, will be taking complicated drug regimens, probably forever, always being followed by the doctor, always having blood tests, always having a little trouble here or there, but alive, and that was a goal that we thought was almost unachievable ten years ago or five years ago. it was in '84 they told me, "we have nothing we can do for you. there are no treatments." but dr. levine said, "your mission, should you choose to accept it, is to try and stay alive as long as you can for us to find a way to treat this," and that's what i set out to do. the death rate due to aids continues to decline as a result of more sophisticated testing
3:46 pm
and treatment. but what many people forget is that the incidence of h.i.v. infection-- that is, the number of people that are infected with the virus here in the united states-- continues to increase, and it's increasing quite rapidly. it's increasing both in the populations that are traditionally at risk, but also in other populations-- in women, in minorities, in young people, adolescents. at the beginning of the epidemic, it was almost unheard of for a woman to have this disease. at this point, though, in the range of 25% of patients with aids are women, and women are the fastest-rising new group of h.i.v./aids in the country, and probably in the world as well. so even people that are in monogamous-- or what they believe are monogamous-- relationships may be at risk if they don't know truly what their partners are involved in. i.v.-drug-use population has become significantly impacted with h.i.v.,
3:47 pm
particularly on the east coast. a decade and a half ago, in atlanta, georgia, sandra mcdonald began to campaign against aids, enlisting the help of those who themselves are h.i.v.-positive. armed with condoms and bottles of bleach, staff members take to the streets. sandra mcdonald: our staff is very good at the unconditional love piece and reaching people where they are, and they're examples by sight. "man, i been there. sister, please. tch. listen, you know who i am? when i left the corner, you took my spot. that's my spot. i been there, baby. it's all right. you know, you can get better, and even if you're not willing to get better today, now here's some condoms. now, this is the package--" that's the street name for h.i.v.-- "and this what you need to know about the package. got to protect yourself. makes sense." that's probably the best that we do. in the last several years, major progress has also been made
3:48 pm
in decreasing the spread of the virus from an h.i.v.-positive mother to her child. alexandra levine: the transmission rate for h.i.v. in the united states from mother to infant is about 25 to 30%. we can lower it to 8% risk by use of anti-h.i.v. medicines given to the mother during pregnancy, given to the mother by vein during the entire time of the delivery, and then given to the infant for the first week of life or the first month of life. progress against the disease in many other parts of the world, is not as promising. it's decimating populations in parts of central africa, in parts of southeast asia, in parts of the indian subcontinent, and it's affecting whole generations of individuals. we know, for example, that there are probably about 25 to 30 million people in the world
3:49 pm
infected with h.i.v. this year, and that that number will continue to increase quite rapidly in the next few years, especially in those parts of the world where prevention efforts and treatment are very minimal. david bennett: the impact of h.i.v./aids in africa has been incredible. to lose the young people who are really the productive segment of society, so that you now have grandmothers who are looking after grandchildren because the adults have disappeared. so a tremendous burden. florence mwayopa: these are some of the children that belong to this household. they are being looked after by their great-grandmother. the... grandmother had twelve children she has lost all except for two. as i traveled to other nations in the world, and especially resource-poor areas of the world,
3:50 pm
one of the things that i'm struck with most is that they are exactly where we were 15 years ago at the very beginning of the epidemic. the first point is that most government officials don't understand what's ready to hit them. one problem that haunts the public health community is how to attack the epidemic as it is spreading through major population areas. there was an international conference on h.i.v./aids in geneva, switzerland, a year ago. the title of the conference was "bridging the gap." under no circumstance were we bridging a gap because on one side of the hall were all of the western countries talking about the side effects of these drugs and how to make it easier for the patient to take the medicines. and on the other side of the hall was the entire rest of the world who had not one concept
3:51 pm
that they would have the ability to have those drugs at all. ronald mitsuyasu: in most countries, they just cannot afford these medications. here in the united states, it's estimated that a year's worth of anti-h.i.v. drugs will cost anywhere between $10,000 and $15,000, and in many parts of the world, their entire health-care budget for a nation will be less than $100 or $200 per person. there's an additional problem which is equally, if not more serious, to my mind. and that these drugs are so difficult to take. in order for them to be effective, they really must be taken... very carefully, according to very strict schedules. they have to be taken in combination. they're not drugs that you can sort of casually take. "oh, i forgot my drug this morning. i'll take it this afternoon or this evening." does not work that way. if that happens, they become ineffective in terms of treating, and it's very, very likely that the usefulness of these drugs
3:52 pm
could be compromised if they're widely used in an incorrect fashion. the resistant virus can be transmitted to somebody else. and we are starting to see, around the world, somebody who has a brand-new infection by h.i.v., and their brand-new virus is already resistant to many of the drugs that we've been using, because the last person who had that virus was resistant and transmitted it. as developed countries are managing the disease more effectively, there is concern among public health officials that their sense of urgency will diminish. we're in danger of thinking about aids in africa and latin america and southeast asia the way we show concern about malaria or epidemic diarrhea or problems of resistant tuberculosis in these same regions of the world. we forget what really made our concern about aids special and that it was a global concern.
3:53 pm
there is an urgent-- a very, very urgent need to develop a vaccine against h.i.v., not only to protect the billions of people in the world that are currently alive, but those who will become alive, and those who will live through the next century. the development of a vaccine is proving to be a very challenging task. harold varmus: it's clear that the aids virus, when it naturally infects the body, does not induce a sufficient immune response to eliminate the virus on its own. that's a daunting prospect for someone who wants to develop a vaccine. secondly, we have a very poor understanding of what components of the virus might be the most potent in inducing a response. i do think it will be a long time before we have an adequate vaccine. alexandra levine worked with jonas salk on what was to be his last major project: looking for a vaccine for h.i.v./aids.
3:54 pm
if the virus could be altered in some way so that it was seen as foreign by the defense system, then perhaps a patient who was already infected could be vaccinated with this altered h.i.v., forcing his immune system to see it and try to destroy it. that was dr. salk's original thought. he was driven to solve this in the same sense that he was driven to solve the polio issue. those ideas are still current. i do believe that we'll have better ways to deliver the so-called antigens, the immune stimulus, rather than use killed virus, which presents some public health risks. and the issue of whether we'll have vaccines to use during the treatment of disease, i think, is still a moot point, but it's one that's being tested in that situation and many others. and we, i think, need to push forward even with vaccine candidates that don't seem as promising
3:55 pm
as, say, the polio virus vaccine is, because those vaccines have been extraordinarily effective. they've allowed us to eliminate the disease entirely, and i think we have to acknowledge the fact that we would have a big impact, even if a vaccine was 50% protective. knowing that a vaccine may be years away, what can we do now to lessen the devastating impact this disease has on people's lives? so the way to protect yourself against h.i.v. is to, number one-- know your sexual partner. know that you are in a monogamous relationship with an h.i.v.-negative person, or abstain from sexual intercourse, or always, always use a condom 100% of the time, a good, clean condom that is not in somebody's pocket for the last 10 years before he takes it out, doesn't have a tear on it. it's a good condom, it's used properly. second way not to get h.i.v. is not to use needles,
3:56 pm
and clearly, not to use needles that are shared with somebody else. you must understand the importance of you. you must understand that for once, you can be selfish and self-centered about your life. when two people engage in sex, it's two people engaging in it. you have the right to protect yourself. we also need to engage young females and males very early on so it becomes a part of their norm. this i how we have sex, protectedly. we either don't have sex, which is wonderful, or if we ever gonna think about it, we do it protectedly. we do it with protection. our capacity to do something about it, particularly our capacity to prevent it, depends upon awareness of the problem at many levels: awareness at the community level, awareness at the national level, and awareness at the individual level. 15-1/2 years ago, they told me that i had 8 months left to live, so i set to work
3:57 pm
to do everything i could to be well, and to stay as well as i could. and it really... it became my mantra to live with aids. then later on, after i got well, i began to think about, "gee, maybe it's possible to live through aids." it is not killing me. it is not interrupting my life. i am living life with the virus inside me, but i am living through it. and in the last couple of years, i've made another transition into living beyond aids. none of us have any guarantees about tomorrow, whether we have h.i.v. or not. all any of us have is right now. so right now, each moment, i can decide to perience the fullness of life, to experience joy, to experience the wonderful communion of talking and sharing and looking in another person's eyes and seeing their soul, and hopefully, their seeing mine.
3:58 pm
3:59 pm
[♪...] >> female announcer: some dreams are universal... dreams that inspire us. multiple sclerosis is a devastating disease that changes lives forever. the national ms society does more for people with ms than any organization in the world... but we can't do it alone. to get involved, visit us online at nationalmssociety.org or call 1-800-fight ms. this is why we're here... because nobody dreams of having multiple sclerosis.
149 Views
Uploaded by TV Archive on

 Live Music Archive
Live Music Archive Librivox Free Audio
Librivox Free Audio Metropolitan Museum
Metropolitan Museum Cleveland Museum of Art
Cleveland Museum of Art Internet Arcade
Internet Arcade Console Living Room
Console Living Room Books to Borrow
Books to Borrow Open Library
Open Library TV News
TV News Understanding 9/11
Understanding 9/11